[Background of study]
Currently, epidemiologic evidence used to guide current physical activity relies heavily on self-reported estimates of leisure-time physical activity or aerobic MVPA and is prone to recall bias and measurement error. Device-based physical activity metrics can more accurately capture sporadic activity of varying intensities throughout the waking day.
Previous studies illustrate that higher duration of physical activity and/or duration of MVPA is associated with lower risk of new-onset cvd. However, it is unclear whether the accumulation of large amounts of light-intensity physical activity (e.g., “hanging out”) or short periods of high-intensity physical activity (e.g., “athletes” or “active commuters”) is associated with a lower risk of new-onset cvd. Are there similar cardiovascular health benefits between the same amount of physical activity?
Elucidating these relationships is challenging because total PA is intensity multiplied by time, making total volume and intensity intrinsically linked as a nested structure (i.e., total volume includes intensity). This implies that alternative analytic approaches to purely time-based physical activity exposures are necessary when examining integrated intensity/volume associations.
[Purpose of the study]
The team previously proposed a methodology to account for the nested nature of intensity in the aggregate by simultaneously analyzing the amount of physical activity and by the proportion of total activity accounted for by moderate- to vigorous-intensity physical activity (MVPA). And it was found that the higher contribution of moderate- to vigorous-intensity physical activity may play a role in the risk of all-cause mortality for a given amount of physical activity; however, it is not clear whether this also applies to cardiovascular disease incidence.
The intensity of physical activity may play a specific role in cardiovascular disease risk compared with the amount of physical activity, possibly due to greater stimulation and adaptation of cardio-related pathways.
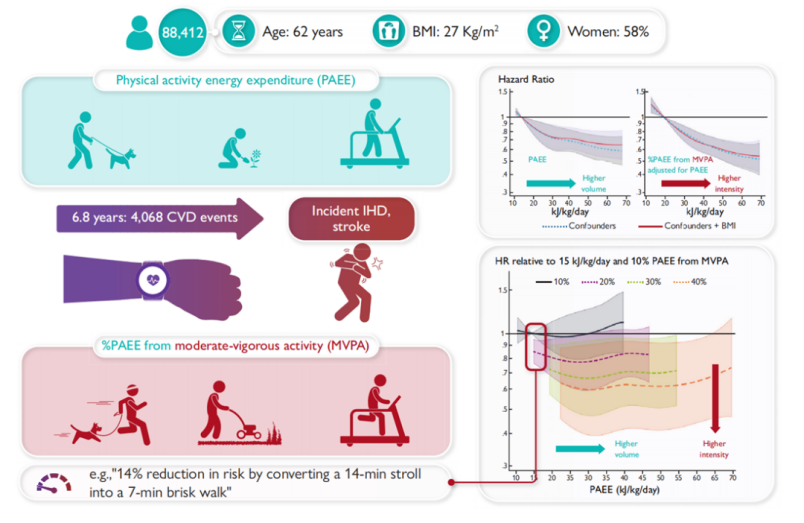
STUDY OBJECTIVE: To investigate the association of device-based estimates of physical activity volume and different levels of physical activity intensity with the onset of new cardiovascular diseases in UKB.
[Analytic Ideas].
1, The relationship between the interaction between the amount and intensity of physical activity (PA) and the risk of cardiovascular disease (CVD) is unknown.
2, Analyze the relationship between PAEE and MVPA as % of PAEE and new-onset CVD separately
3, Analyze the interaction between PAEE and MVPA as % PAEE
4, Analyze the stratified stratification by gender
[Methods]
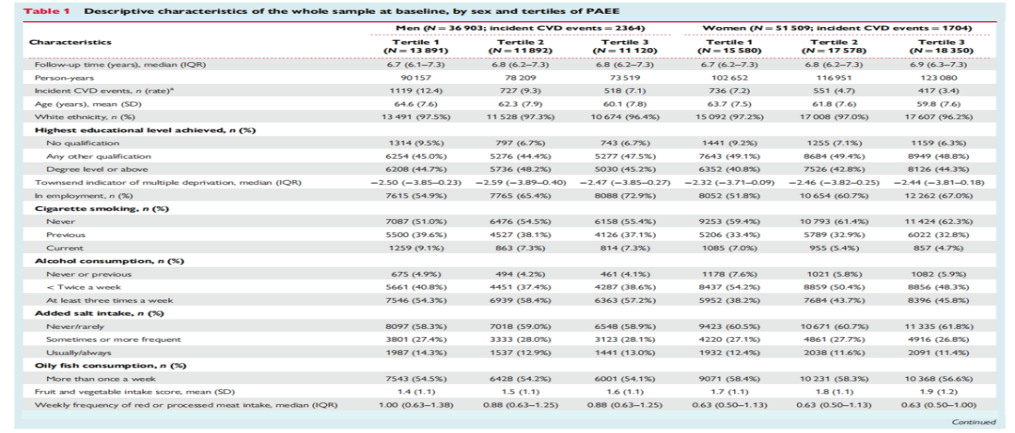
Subjects: 88,412 middle-aged adults in UKB with a median follow-up of 6.8 years Total amount and intensity of PA: wrist tri-axial accelerometers were worn for 7 days, and instantaneous physical activity energy expenditure (PAEE) was estimated based on the intensity of wrist movements
Total: (i)Average daily physical activity energy expenditure (kJ/kg/day) – calculated as the sum of physical activity-based energy expenditure for all intensity levels;
Intensity: (ii) Proportion of physical activity-based energy expenditure for moderate to vigorous intensity physical activity (%MVPA)-calculated as the sum of energy expenditure for all activities greater than 3(MET) of the total energy expenditure of all activities divided by the total physical activity energy expenditure.
Outcome: new-onset nonfatal/fatal CVD was defined as the first occurrence of ischemic heart disease or cerebrovascular disease.
Covariates: demographic and lifestyle-related characteristics: age, gender, race, Townsend Index (based on zip code), highest level of education, employment status), parental history of cardiovascular disease or cancer, season of accelerometer wear, alcohol consumption status, salt addition, intake of oily fish, intake of fruits and vegetables, intake of processed and red meats, sleep duration, and whether they were diagnosed with cancer before baseline.
Health-related covariates: blood pressure or cholesterol medications, insulin prescription or self-reported physician-diagnosed diabetes, mobility limitations (self-reported long-term illness or disability or chest pain at rest), and body mass index (BMI).
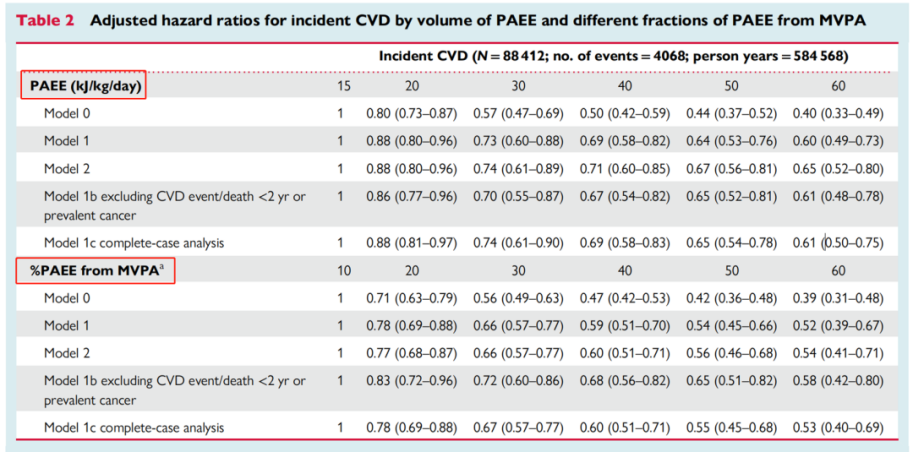
Using Cox proportional risk regression models, we first examined the association of PAEE and the score of PAEE in MVPA (the latter corrected for PAEE) with new-onset CVD.
These models used age as the underlying time scale and modeled exposures using cubic spline and three evenly spaced nodes.Model1: was the primary confounder-corrected model and was further corrected for race, education level, employment status, Townsend index, dietary variables, alcohol consumption, smoking status, mean sleep duration, parental history of CVD or cancer, blood pressure or cholesterol medication use, diabetes diagnosis or insulin prescription, mobility limitations, and common cancers.
Model 2: Corrected for body mass index, which may be considered a potential confounder but also a potential mediator between physical activity and new-onset CVD, given that there appears to be a bidirectional association between body mass index and physical activity.
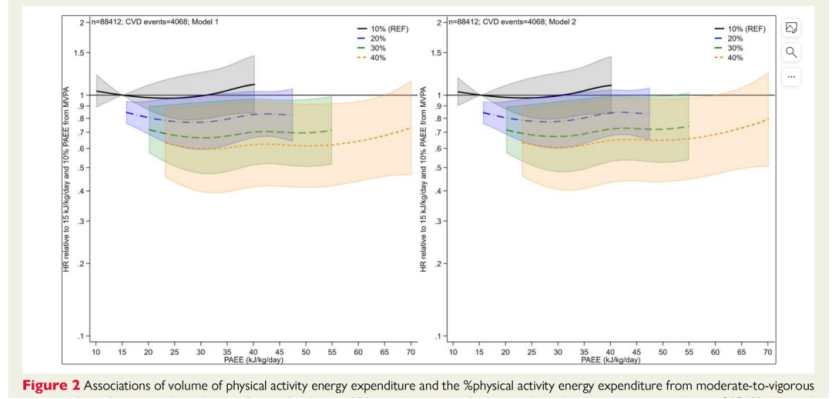
In examining the interaction between physical activity amount and intensity, PAEE and log-transformed %PAEE from MVPA were fitted using spline regression, which included four orthogonal spline variables and an interaction term between %PAEE. Using the coefficients, we plotted the fitted spline function showing the association between PAEE and cardiovascular disease risk for the incremental components from MVPA (10%, 20%, 30%, and 40%).
Sensitivity analysis: no fill analysis; excluded samples with new CVD within 2 years of follow-up; used 2 other parameters instead of PAEE and MVPA as % of PAEE to do the relationship with CVD occurrence. (strong correlation)
[Findings] Baseline characteristics: by sex and PAEE tertiles
After correction for potential confounders and cancer prevalence (model 1), both higher PAEE and % PAEE of MVPA (corrected for PAEE) were negatively associated with the incidence of new CVDs