On March 31, 2025, at the European Heart Rhythm Society 2025 meeting in Vienna, Austria, Dr. Tobias Reichlin of the University of Bern, Switzerland, reported the results of the head-to-head comparison of pulsed-field vs. thermal ablation for the treatment of paroxysmal atrial fibrillation in the noninferiority SINGLE SHOT CHAMPION trial, which was simultaneously published in the New England Journal of Medicine (NEJM) published online. The findings show that in patients with paroxysmal atrial fibrillation, the use of pulsed-field ablation (PFA) is noninferior or even slightly superior to cryoballoon pulmonary vein isolation (PVI) in preventing arrhythmia recurrence.
The NEJM published the results of the multicenter, noninferiority ADVENT trial of pulsed-field vs. thermal ablation for paroxysmal AF in 2023, which demonstrated that in patients with paroxysmal AF, pulsed-field ablation was associated with a composite of procedural success, atrial tachyarrhythmias after a 3-month blanking period, use of antiarrhythmic medications, cardioversion, or repeat ablation, as compared with conventional thermal ablation, as well as a composite of device- and procedure-related serious adverse events within 1 year. Pulsed-field ablation was noninferior to conventional thermal ablation in terms of device- and procedure-related serious adverse events within 1 year.
What are the new findings of the SINGLE SHOT CHAMPION trial relative to the ADVENT trial? We present the results of that study here.
Atrial fibrillation (AF) is the most common cardiac arrhythmia, with a population prevalence of 1% to 2%. AF not only affects patients’ quality of life, but also increases the risk of complications such as heart failure and stroke. Catheter ablation has become the standard treatment for AF. However, catheter ablation faces two major challenges: suboptimal efficacy (paroxysmal AF has a success rate of 67% to 74% 1 year after ablation) and safety issues (pulmonary vein stenosis, phrenic nerve palsy, and arterioesophageal fistulae, which can lead to death). As a nonthermal therapy, pulsed field ablation (PFA) uses microsecond high-voltage electric fields that can cause myocardial cell membrane instability and electroporation, which can lead to cell death. Pulsed field ablation is highly effective in eliminating arrhythmias and is selective for the targeted myocardium without causing collateral damage to surrounding tissues.
The previous ADVENT trial has shown that in patients with paroxysmal atrial fibrillation, PFA is comparable to radiofrequency or cryoablation in terms of efficacy and safety, and the procedure time is shorter. Although the results of that study were consistent with observational studies, none of the studies used continuous rhythm monitoring to fully assess recurrence rates and AF load.
The SINGLE SHOT CHAMPION trial was conducted in two tertiary care centers in Switzerland, operated by experienced operators, and enrolled 210 patients with symptomatic paroxysmal atrial fibrillation (mean age 64 years, 28% female) who were randomly assigned to receive either PFA or cryoballoon for first pulmonary vein isolation (PVI). All patients were implanted with a rhythm monitor for postoperative arrhythmia monitoring. Repeat ablation was not allowed during the 3-month postprocedure blanking period, during which antiarrhythmic drugs could be used but then had to be discontinued.
The mean procedure time was shorter in the PFA group (55 min vs. 73 min), and fluoroscopy time was similar (14.6 min vs. 15.1 min.) Higher high-sensitivity troponin levels were seen in the PFA group after the procedure (1,920 ng/L vs. 1,114 ng/L).
The difference in the rate of first recurrence of atrial arrhythmias between 91 and 365 days after surgery was -13.6% (95% CI, -26.9% to -0.3%; P for noninferiority <0.001; P for superiority = 0.046), which met the criterion for noninferiority (upper confidence interval lower than 20%). When considering the overall one-year postoperative period, the difference in recurrence rate was -18.2%. The difference between the two ablation modalities was most significant within the first 90 days, perhaps indicating that different mechanisms of cardiac injury can influence the pattern of cardiac recovery.
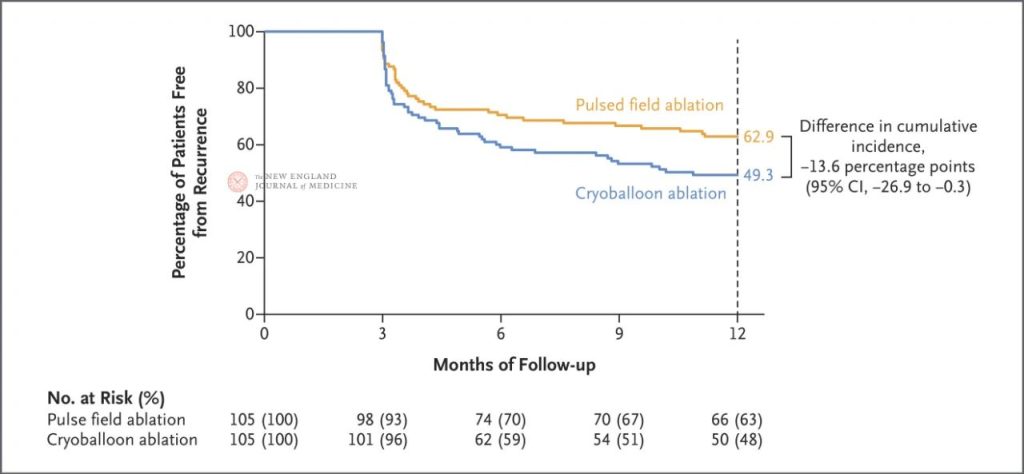
Kaplan-Meier estimates of the percentage of patients with no recurrence of atrial tachyarrhythmias (primary end point) from 91 to 365 days after ablation (i.e., after a 90-day blanking period). The estimates of no recurrence at 365 days for the pulsed-field ablation group and the cryoballoon ablation group were 62.9% and 49.3%, respectively, which corresponded to 100% minus the cumulative incidence in both groups.
During the blanking period, the mean atrial arrhythmia load was lower in the PFA group than in the cryoablation group (a difference of -2.4%); however, the difference between the two groups narrowed to -0.5% and was no longer significant between days 91 and 365.
The primary safety endpoint, procedure-related complications within 30 days, was less frequent in both groups: 1 mild stroke in the PFA group and 2 cardiac pressures requiring drainage in the cryoablation group. 1 additional patient in the PFA group died of cancer 11 months after the procedure.
The number of hospitalizations or emergency room visits due to recurrent atrial arrhythmias was less in the PFA group than in the cryoablation group (2 vs. 8), but the difference was not significant.The rate of repeat ablations after the postprocedure blanking period was slightly higher in the PFA group (15.2% vs. 9.5%), but the difference was also not significant. Quality of life scores (EQ-5D-5L scale and visual analog scale) were comparable between the two groups at 3 and 12 months.
Limitations of this study include: the trial used only one PFA system, and the results may not be generalizable to other techniques; data on preoperative AF load are lacking; and the study was conducted in only two experienced centers, and extrapolation needs to be validated.
PFA Application Trends and Outlook
There are important differences between the SINGLE SHOT CHAMPION trial and the previous ADVENT trial. The latter had a larger sample size and more centers, but used only intermittent monitoring to determine recurrence of AF. The SINGLE SHOT CHAMPION trial, on the other hand, used continuous rhythm monitoring and thus was more accurate in determining arrhythmia recurrence.
In the SINGLE SHOT CHAMPION trial, the rate of first recurrence of atrial arrhythmia was lower in the PFA group, but because the statistical significance of the test of superiority was just below the standard, data bias in a few patients could change the results. Therefore, the superiority of PFA in this trial should not be overinterpreted at this time.
The higher rate of repeat ablation in the SINGLE SHOT CHAMPION trial compared with the ADVENT trial may be related to the higher sensitivity associated with continuous monitoring, suggesting that future trials should be designed with the caveat that more frequent monitoring may inadvertently lead to more procedures.
With regard to safety, although the number of serious adverse events is low, the percentage cannot be ignored due to the small overall inclusion.The ADVENT trial has reported asymptomatic brain injury in the PFA group, which is a reminder of the need to remain vigilant before the technology is promoted as a first-line tool.
Despite these issues, these findings support the use of PFA as a first-line treatment for paroxysmal AF. Future studies should assess AF load both before and after ablation as a central indicator of treatment success rather than relying on the presence or absence of transient AF episodes.



