In public perception, hypertension and dementia seem to be two distinct diseases. However, a growing body of medical research is revealing the inextricable link between them.
An important study published in Nature Medicine (IF=45.78), a top international journal, confirms that intensive antihypertensive treatment for hypertensive patients can effectively reduce the risk of dementia. This discovery brings a brand new idea and direction to the global hypertension and dementia prevention and treatment field.
How can clinical treatments break the ice and find their way as the global burden of dementia disease increases?
Currently, the global dementia disease burden is growing at an alarming rate. According to statistics, the number of dementia patients worldwide has reached 57.4 million in 2019, while it is expected that by 2050, the number will soar to 152.8 million. As the fifth leading cause of death globally, dementia causes about 2.4 million deaths each year, which not only seriously threatens the lives and health of patients, but also imposes a heavy financial and emotional burden on family caregivers and society.
Regrettably, the medical community still lacks effective therapies that can cure dementia. Against this backdrop, primary prevention of dementia by eliminating risk factors has become an urgent priority in public health. A large number of observational epidemiologic studies have clearly indicated that hypertension, age, and genetics are important risk factors for dementia, among which hypertension, as an interventable risk factor, is particularly worthy of attention and in-depth research on its association with the onset of dementia.
As a common chronic disease, hypertension is an important modifiable risk factor for cardiovascular disease and premature death. Prolonged hypertension can significantly increase the risk of dementia through a variety of mechanisms, including damage to cerebral blood vessels, cerebral blood perfusion, and cerebral white matter lesions. Previous studies have tentatively suggested that antihypertensive treatment may reduce the risk of dementia in hypertensive patients. However, there are significant limitations in the existing studies. For example, most of the studies were conducted in non-demented populations, making it difficult to accurately reflect the true risk in hypertensive patients; at the same time, some of the studies were conducted with small sample sizes and flawed study designs, resulting in a low level of evidence and making it difficult to form reliable clinical recommendations. Therefore, high-quality clinical studies are urgently needed to provide solid evidence-based medical support for dementia prevention in hypertensive patients.
Research Breakthrough: World’s Largest Study of Blood Pressure Reduction to Prevent Dementia Unveiled
Compared with previous studies, this study achieved a major breakthrough in study design and sample size, providing strong evidence-based evidence for antihypertensive treatment to prevent dementia. The study is the world’s largest whole-cluster randomized controlled study of antihypertensive treatment for the prevention of dementia. 33,995 hypertensive patients were enrolled and randomly assigned to a comprehensive intervention group (n=17,407) with an intensive antihypertensive regimen targeting 130/80 mmHg, and a conventional hypertension management strategy in the conventional management group (n=16,588).
In order to investigate the effect of intensive antihypertensive on dementia prevention, the research team conducted an in-depth analysis from multiple dimensions, including blood pressure control, medication use, dementia and related outcomes, and serious adverse events.
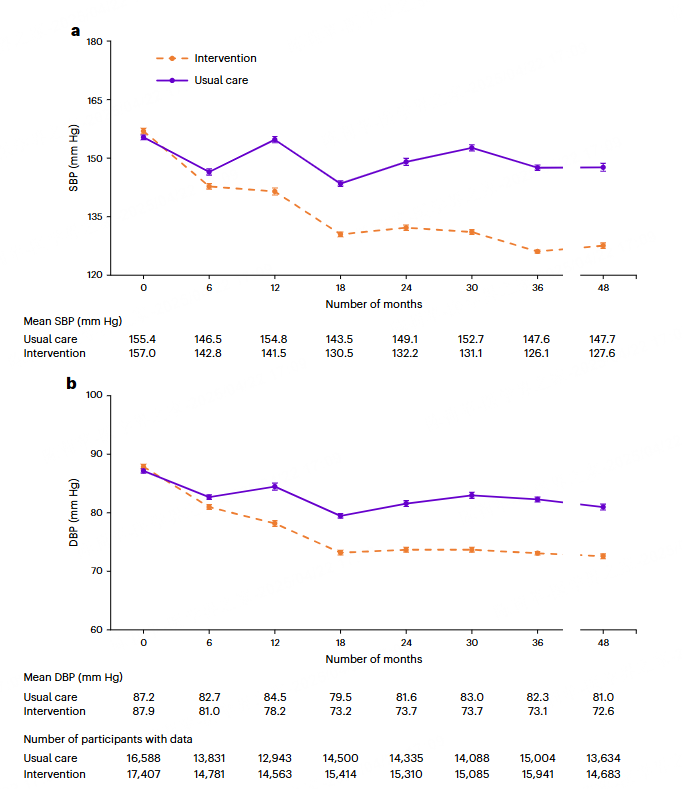
I. Blood pressure control: intensive antihypertensive significantly better than conventional management
Patients in the intervention group had a baseline systolic blood pressure (SBP) of 157.0±18.0 mmHg and a diastolic blood pressure (DBP) of 87.9±10.9 mmHg, which decreased to 127.6±12.8 mmHg and 72.6±8.3 mmHg at 48 months, resulting in a significant reduction in blood pressure. In contrast, SBP decreased from 155.4±17.4 mmHg to 147.7±20.2 mmHg and DBP from 87.2±10.7 mmHg to 81.0±11.3 mmHg in patients in the routine management group, which was a much lesser decrease than that in the intervention group, although there was a decrease in blood pressure.
The data showed that the net difference in SBP between patients in the intervention group and those in the conventional management group amounted to -22.0 mmHg (95% CI: -23.4 to -20.6, P<0.0001), and the net difference in DPB was -9.3 mmHg (95% CI: -10.0 to -8.7, P<0.0001) over the 48-month period. Moreover, at 48 months, 67.7% of the patients in the intervention group achieved the ideal BP goal of SBP<130 mmHg and DBP<80 mmHg, whereas only 15.0% of the patients in the conventional management group met the goal. This fully demonstrates that the intensive antihypertensive program has obvious advantages in blood pressure control.
II. Drug Use: More Aggressive Treatment Strategies Aid Blood Pressure Management
In terms of antihypertensive drug use, the two groups showed significant differences. 48-month follow-up results showed that patients in the intervention group were taking an average of 3 antihypertensive drugs (95% CI: 3.0~3.1), compared with only 1.2 drugs in the conventional management group (95% CI: 1.1~1.2, P<0.0001 for the difference between groups).
In terms of specific drug categories, the proportion of angiotensin-converting enzyme inhibitors (ACEIs), calcium channel blockers (CCBs), and diuretics in the intervention group was 50.3%, 86.8%, and 63.8%, respectively, which was significantly higher than that of the conventional management group, which was 6.3%, 53.3%, and 10.8% (P value < 0.0001 for all comparisons), reflecting a more aggressive drug treatment strategy. However, the proportion of angiotensin II receptor blocker (ARB) use was similar in the two groups (30.1% in the intervention group vs. 32.3% in the routine management group), suggesting that the impact of ARBs on the difference in blood pressure control between the two groups was relatively small.
III. Dementia and related outcomes: intensive blood pressure lowering effective in reducing risk
In terms of the much-anticipated dementia and related outcomes, the study made groundbreaking findings.At 48-month follow-up, the number of confirmed cases of all-cause dementia was 668 (4.59%) in the intervention group and 734 (5.40%) in the conventional management group, and the risk ratio (RR) for all-cause dementia in the intervention group was 0.85 (95% CI: 0.76-0.95, P=0.0035), implying that the intensive antihypertensive intervention significantly reduced the risk of all-cause dementia.
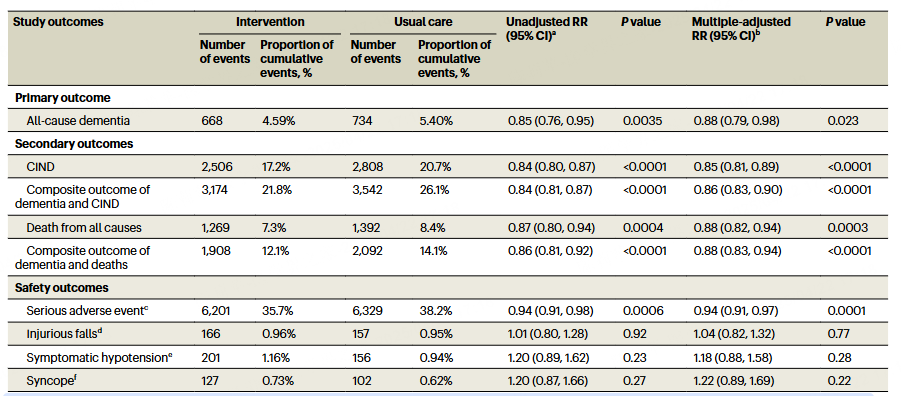
Further analysis of clinical non-dementia cognitive impairment (CIND) showed that there were 2,506 (17.2%) confirmed diagnoses in the intervention group, compared with 2,808 (20.7%) in the routine management group, and the RR for CIND in the intervention group was 0.84 (95% CI: 0.80 to 0.87, P<0.0001). For the composite outcome of dementia or CIND, the RR was similarly 0.84 (95% CI: 0.81~0.87, P<0.0001); the RR for the composite outcome of dementia or death was 0.86 (95% CI: 0.81~0.92, P<0.0001). These data fully confirm that intensive antihypertensive intervention is effective in reducing the risk of adverse cognitive outcomes and associated death.
IV. Safety: Intensive blood pressure lowering did not increase the risk of adverse events
In terms of safety, there were 6201 cases (35.7%) of serious adverse events in the intervention group and 6329 cases (38.2%) in the routine management group, and the risk ratio (RR) of serious adverse events in the intervention group was 0.94 (95% CI: 0.91~0.98, P=0.0006). This suggests that intensive antihypertensive intervention is not only effective in reducing the risk of dementia, but also did not significantly increase the risk of serious adverse events, and has a good performance in terms of safety.
In summary:
This study demonstrates for the first time that intensive antihypertensive treatment for hypertensive patients can significantly reduce the risk of dementia. In a large-scale randomized controlled trial, the study found that intensive antihypertensive therapy not only effectively controls blood pressure and improves compliance, but also reduces the risk of all-cause dementia, cognitive impairment, and related deaths, and has a favorable safety profile. The results provide a new direction for the management of hypertension, and are expected to promote the updating of clinical diagnosis and treatment guidelines, and assist in early intervention and precision prevention and treatment. In the future, we look forward to more studies exploring the best strategies for intensive antihypertensive treatment, which will provide stronger support for reducing the global burden of dementia.



