“Doctor, I started using inhalers after I was diagnosed with cough variant asthma, but I still tend to have a dry cough every change of season, especially after exercise when the symptoms are more pronounced, why is that?” A viewer in the broadcasting room said the common confusion of many patients.
Many friends believe that as long as the medicine is sufficient, not realizing that environmental control, drug selection in a number of aspects of the invisible misunderstanding may make the efficacy of greatly reduced.
Myth 1: Thinking that if you create a clean space, you won’t have an asthma attack
- “Cough variant asthma essentially belongs to a special type of asthma, and patients often have an allergic basis, often combined with other allergic diseases, such as allergic rhinitis or atopic dermatitis, etc.. As the upper and lower respiratory tracts are connected, some patients who originally only have allergic rhinitis may also develop cough variant asthma after the disease progresses.”
- “Patients with a combination of other allergic diseases need to pay special attention to these early warning signs on a daily basis: allergic rhinitis symptoms such as frequent sneezing and runny nose in the morning, or respiratory discomfort aggravated in the spring and fall seasons; recurrent hives on the skin or sudden rashes after contacting allergens; and allergic reactions triggered by certain specific foods (e.g., mango, seafood, etc.). It is worth noting that there are individual differences in allergens, and it is recommended to clarify one’s own sensitizing substances through professional testing.”
- “With the increase in the number of pet-owning families in recent years, it is also important to be alert to delayed allergic reactions triggered by pet hair. Some patients may be exposed to cats and dogs for several months before the gradual onset of coughing symptoms, which may be complicated by allergic rhinitis and asthma in severe cases. Therefore, if you have a prolonged cough and have pets at home, it is recommended to promptly check for allergic factors.”
- As you read this, some of you may ask, “If you could create a completely allergen-free clean space, wouldn’t you be able to avoid asthma attacks?” This wonderful wish is difficult to realize in reality. Asthma, as a chronic respiratory disease, has an attack mechanism that involves multiple factors such as genetics, immunity, and the environment, and simply relying on environmental purification does not solve all problems. What’s more, we can’t live completely apart from the natural environment. Instead of pursuing an unrealistic “zero allergen” environment, it is better to learn scientific prevention.

Myth 2: Take only cough suppressants to relieve symptoms
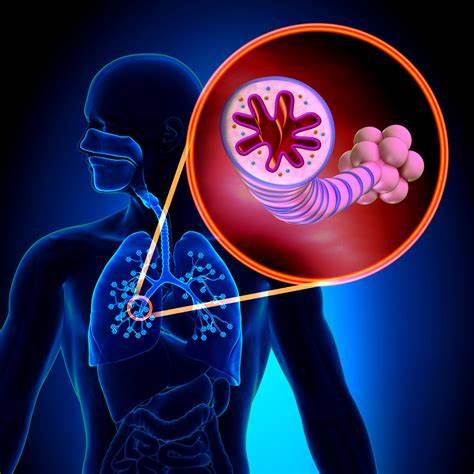
- Some patients believe that as long as the cough suppressants to “suppress” the cough, all is well, in fact, this treatment belongs to the “treatment of the symptoms but not the root cause”. Cough suppressants only inhibit the cough reflex, but the core of cough variant asthma is chronic airway inflammation and airway hyperresponsiveness, not to control the inflammation, cough will recur. In addition, simply suppressing the cough may mask the progression of the disease, leading to the development of cough variant asthma into classic asthma, with more severe symptoms such as wheezing and dyspnea.
- What are the usual treatment options if cough variant asthma is diagnosed? Prof. Zhou told us, “After diagnosis of cough variant asthma, inhaled glucocorticosteroids combined with long-acting beta 2 agonists are usually recommended, which can effectively reduce airway hyperresponsiveness through the dual mechanism of anti-inflammatory and bronchodilator. The treatment cycle needs to last at least two to three months, with the exact course of treatment flexibly adjusted according to the patient’s actual situation, and discontinuation of the drug can only be considered when there is a complete absence of coughing symptoms and lung function has returned to normal. The following year needs to be closely observed for seasonal recurrence so that the treatment program can be adjusted in time.”
- “Alternatively, an oral leukotriene receptor antagonist can be added; montelukast sodium (4-5 mg/night) is commonly used in pediatrics, and the adult dose is 10 mg/day. Patients with severe symptoms may receive oral prednisone for a short period of time (5-7 days) and wait until symptoms resolve before transitioning to inhaled therapy.”
- “It is important to emphasize that medication must be combined with preventive management for optimal efficacy. The first and foremost principle is to block allergen exposure. If you are continuously exposed to sensitizing environments (e.g., dust mites, pollen, or pet hair), it is difficult to achieve the desired therapeutic effect even with standardized medication. Therefore, it is recommended to identify the causative agent through allergen testing and take environmental control measures, such as using mite-proof bedding, maintaining indoor ventilation, and avoiding keeping stuffed pets, in order to minimize the risk of flare-ups at the source.”

Myth 3: Rush for tests after only a week or two of coughing
- If the cough persists for 1-2 weeks, tests such as pulmonary function tests are usually not needed immediately. In most cases, acute coughs are caused by viral or bacterial infections of the respiratory tract, and cough suppressants can be used appropriately. It is also recommended to keep an eye on family members living with you and office colleagues for similar symptoms, and to keep a daily record of the frequency of coughing and any changes in the symptoms, and to seek medical attention if there is a persistent high temperature, chest pain, or difficulty in breathing. If the cough persists for more than eight weeks, consider the following tests:
- “Basic pulmonary function tests are preferred, and a bronchodilator test is required in patients with ventilatory dysfunction (e.g., FEV1 values less than 80% of predicted values). This is done by retesting lung function after inhalation of a short-acting β2 agonist (e.g., salbutamol), which suggests the presence of reversible airflow limitation consistent with asthma if the FEV1 improves by ≥12% and increases by an absolute value of ≥200 ml after administration.”
- “Patients with normal baseline lung function but high clinical suspicion of asthma need to undergo a bronchial provocation test, which involves observing the magnitude of the decrease in FEV1 after inhalation of a stimulus such as acetylmethacholine by nebulization, and when the decrease is ≥20% it can be determined as positive airway hyperresponsiveness, which can also lead to a diagnosis of asthma.”
- “During pulmonary function testing, it is recommended to synchronize the completion of exhaled gas nitric oxide (FeNO) measurement, a noninvasive test that reflects the level of airway inflammation by detecting the concentration of nitric oxide in exhaled gas, with elevated values suggesting eosinophilic airway inflammation, which is of high diagnostic value and is applicable to patients of all ages.”
- “In addition, it is recommended that routine blood tests be completed during the stabilization period to assess eosinophil levels, an elevation of which is usually indicative of an allergic reaction state. Allergen screening can also be performed, and there are currently two main tests available, serum-specific IgE testing and skin prick testing.”




