Transcatheter arterial embolization (TAE) therapy has evolved dramatically over the past half century. Guided by real-time imaging equipment, embolic agents and embolic devices can be guided through the catheter from superficial vessels to the target vessels deep in the body, transforming the originally complex open surgery into a minimally invasive procedure with fewer complications and lower-cost embolization.TAE aims to block the blood flow of the target vessels, and it is suitable for tumors, hemorrhagic lesions, aneurysms, and vascular malformations. In the field of tumor treatment, transcatheter arterial chemoembolization (TACE), which combines embolization and chemotherapy, is recognized both domestically and internationally as the treatment technique of choice for intermediate and advanced hepatocellular carcinoma (HCC). At present, a variety of embolization products, including solid embolic agents, liquid embolic agents and embolization devices, have been applied in clinical treatment. With the development of material science, shape memory foam, in situ gel, degradable polymers, and micro-robotics have also been studied and applied to embolization therapy.
- solid bolus
Solid suppositories are by far the most commonly used type of suppository and can be categorized into particulate and microsphere types. Compared to irregular particulate type embolizers, calibrated microspheres have rounded surfaces and regular shapes with a strict range of particle sizes. Selection of microspheres with the appropriate particle size based on the type of disease and clinical need can reduce the risk of ectopic embolization. Compared with conventional TACE, drug-loaded microsphere TACE can effectively embolize blood vessels and release drugs slowly, and has been studied and applied in all stages of HCC treatment in recent years.
- Non-degradable
PVA type:
PVA polymer is a poorly degradable and biocompatible material that can be used as a long-lasting embolic agent. After crushing and sieving, PVA embolic particles of different sizes can be obtained. However, PVA embolic particles lack size precision and are easy to aggregate, which can easily block catheters and ectopic embolization, while rationally designed PVA microspheres with regular shape, good morphology, good water absorption and expansion properties and good embolization effect are widely used in the clinic. Most of the clinically used embolic agents lack visualization properties, and interventionalists usually need to physically mix them with contrast agents. However, embolic agents are easily separated from the contrast agent and are difficult to review after the procedure.Negussie et al. successfully synthesized contrast microspheres based on DC Bead, a sulfonate-modified PVA microsphere, chemically conjugated with 2,3,5-triiodobenzenemethanol, which provided real-time feedback on the location of the microspheres and the degree of embolization.
Professor Yang Guang’s team developed a multifunctional embolization microsphere (BaSO4/PVA/CS microsphere) loaded with both thrombin and BaSO4 nanoparticles, which combines both development and local procoagulant functions, enabling precise localization during embolization. After tumor embolization, secretion of vascular endothelial growth factor (VEGF) induces an angiogenic response that limits the therapeutic efficacy of the treatment.Sakr et al. loaded an anti-VEGF antibody (bevacizumab) onto a DC Bead and controlled the release kinetics by alternately coating it with alginate and polylysine. that the microspheres have the potential to improve tumor therapeutic efficacy. In addition, improving the hypoxic microenvironment after TACE is another strategy to inhibit tumor regeneration.Chen et al. developed a multifunctional PVA/hyaluronic acid microsphere (PT/DOX-MS) combining DOX and PT-2385, a selective HIF-2α inhibitor, for the enhancement of TACE treatment. It was shown that PT/DOX-MS could block tumor cells at G2/M phase, promote apoptosis and inhibit tumor angiogenesis.The anti-tumor mechanism of PT/DOX-MS may be that PT-2385 could effectively inhibit the HIF-2α expression level in hypoxic HCC cells, which in turn down-regulated the expression levels of Cyclin D1, VEGF and TGF-α. In addition, the combination of DOX and PT-2385 could jointly inhibit VEGF expression.
PEGs:
PEG is a polymer consisting of ethylene glycol monomers, which has good water solubility and biocompatibility, but is difficult to degrade in the organism. As a hydrophilic material, PEG maximizes suspension time and has good transcatheter delivery properties. A retrospective study found that among 42 HCC patients who underwent TACE (using DOX-loaded PEG microspheres), all patients tolerated TACE well, with no surgery-related complications or systemic drug-related adverse events, and that at 6 months of treatment, the patients had a tumor remission rate of 43% in complete remission, a partial remission rate of 19%, a lesion stability rate of 29%, and a lesion progression rate of 10%, suggesting that PEG microspheres are effective and safe. Another study demonstrated that TACE using epirubicin-containing PEG microspheres is technically feasible, safe, and effective for the treatment of HCC.Li et al. synthesized and fabricated a radiopaque microsphere encapsulated with iodine oil using a multiblock copolymer-based urethane of PEG and polycaprolactone, which demonstrated highly effective in vivo embolization.PEG microspheres are difficult to degrade and are often only used for permanent embolization. Currently, researchers are focused on introducing degradable components into PEG microspheres to obtain PEG embolization microspheres that can be degraded in vivo.
- Biodegradable
Autologous source category:
Blood clots, subcutaneous tissue, and muscle fragments of autologous origin have been used as embolic materials in the past, and the first attempt at embolization was made in 1970 by Charles Dotter’s team, who used an autologous blood clot as an embolic agent to control gastric ulcer hemorrhage in a critically ill patient by selective embolization of the right gastric omental artery. Although embolic materials of autologous origin are obsolete, their demonstrated degradability and less inflammatory response provide ideas for the development of embolic materials.
Gelatine:
Non-biodegradable embolic agents often lead to severe inflammatory reactions and hinder subsequent treatment, so embolic materials with biodegradability and imaging capabilities have attracted much attention. Gelatin-based embolic agents are biodegradable and mainly include gelatin sponge blocks, gelatin sponge particles and gelatin microspheres. Gelatin sponges are usually mixed with contrast agents to form an injectable slurry for in-treatment imaging purposes.Ye et al. tightly embolized adult New Zealand rabbit renal arteries with gelatin sponge particles (150-350 μm) and found that the particles were degraded and absorbed by day 14; vascular recanalization occurred after degradation of the gelatin sponge, but intimal hyperplasia leading to permanent vascular occlusion was observed after day 28.Zhao et al. found that embolization of HCC patients without surgical resection using gelatin sponge particles was safe, effective and had a better prognosis.
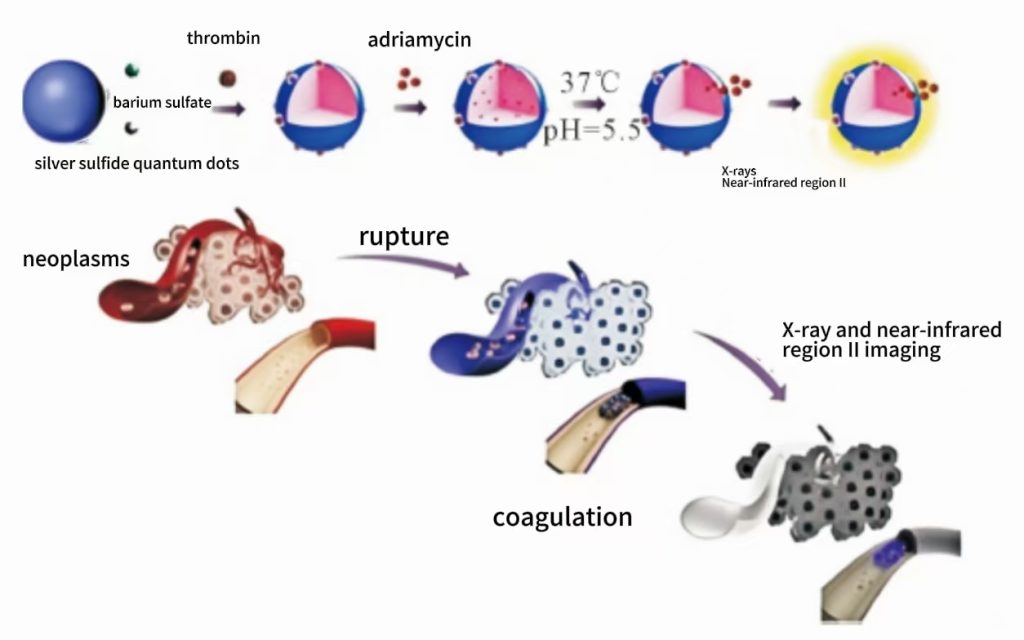
However, it has also been shown that gelatin particles (40-60μm) may undergo distal migration, which increases the risk of ischemic tissue or nerve injury.Gao et al. prepared gelatin microspheres encapsulated with silver sulfide quantum dots and BaSO4 (Fig. 1), which had good NIR 2-region imaging and X-ray imaging capabilities, breaking the limitation of traditional embolization microspheres that are only available for X-ray imaging, and in addition, can be combined with thrombin and DOX to improve the therapeutic effect on tumors; experiments showed that the microspheres had a good embolization effect on both ear and renal arteries of New Zealand white rabbits. Overall, gelatin-based embolic agents have shown good results in the treatment of uterine fibroids, liver tumors and bone malignancies. However, their degradation properties are unpredictable and the embolization process may lead to an earlier recovery of blood flow, making them unsuitable for permanent embolization.
Hyaluronic acid:
The hydroaluronic acid, HA, is a natural hydrophilic polysaccharide with superior biocompatibility and degradability.Yi et al. developed a “one-step solution drying technique” to cross-link the HA microspheres with 1,4-butanediol diglycidyl ether, and introduced BaSO4 nanoparticles to improve the imaging ability of the microspheres. Imaging ability. The microspheres were non-cytotoxic and better hemocompatible, and could be tracked and identified in real time during TACE. In addition, histopathological analysis and CT images confirmed that the HA microspheres had an effective embolic vascularization and visualization ability for at least 4 weeks. This technique yields monodisperse HA microspheres with diameters ranging from 350 to 900 μm, consistent with the standard distribution of commercial embolic microspheres. Unfortunately, however, there are no commercially available embolic products of HA microspheres that can be used for embolization.



